What is Acute Kidney Injury?
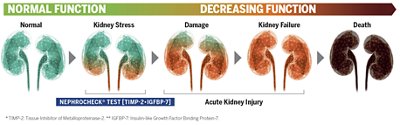
Acute Kidney Injury is an abrupt loss of kidney function that develops within 7 days. It is currently diagnosed using serum creatinine and urine output. It is a frequent syndrome in the ICU, where patients show hemodynamic instability, present various comorbidities, and are exposed to nephrotoxic drugs which put them at risk of developing AKI.
What is the Healthcare Burden of AKI?
Acute kidney injury is an increasing global challenge for patients, healthcare providers, and societies:
- 13.3 million new cases of AKI per year3
- 74% of ICU patients develop AKI1,2
- 42% of septic patients in ICUs have AKI4
AKI is associated with serious short and long-term complications, including longer hospital and ICU stays and increased mortality rates. AKI survivors are also at increased risk of developing chronic kidney disease (CKD) and cardiovascular complications. Greater severity, prolonged duration, and recurrent episodes of AKI amplify its overall impact. Also, when an acute kidney injury progresses to a chronic kidney disease, the patient's well-being, quality of life, and families are all impacted.
Healthcare costs associated with AKI management are high and exceed those of common cancers.5 In the absence of successful therapies to treat AKI, prevention is paramount. Identifying patients at high-risk of AKI provides a window of treatment for the healthcare community.
While tools already exist to diagnose AKI, serum creatinine levels and urine output are lagging indicators in critically ill patients, with low sensitivity and specificity.6 In this setting, AKI is therefore generally diagnosed late.
What is Our Solution for AKI?
bioMérieux has developed an assay that detects kidney stress when intervention can still make a difference. It is intended to be used in acutely ill patients in conjunction with clinical evaluation, to aid in identifying patients at risk for developing moderate or severe AKI within the following 12 hours.
With an early warning, healthcare providers can personalize medicine and confidently rule out patients from nephroprotective measures, or implement nephroprotective measures to improve patient outcomes and reduce costs7,8, and potentially reduce the development of new comorbidities.
Acute Kidney Injury (AKI) – Our Diagnostic Offer
bioMérieux offers one of the only stress biomarkers commercially available to improve AKI management.
Disclaimer: Product availability varies by country. Please consult your local bioMérieux representative for product availability in your country
-
VIDAS® 3
Trusted. Robust. Innovative.
With its advanced immunoassay technology and optimized testing protocols, the fully automated VIDAS® 3 benchtop immunoanalyzer empowers your lab with confidence, offering the precise results you need, when you need them.
-
VIDAS® NEPHROCHECK®
Reveal Kidney Stress Early. Drive Better Outcomes.
VIDAS® NEPHROCHECK® measures urinary TIMP-2 & IGFBP-7, specific urinary biomarkers for early risk assessment of moderate to severe Acute Kidney Injury (AKI). The VIDAS® NEPHROCHECK® assay is intended to be used in conjunction with clinical evaluation as an aid in the risk assessment for moderate or severe acute kidney injury (AKI) in acutely ill patients.
Useful Resources on Acute Kidney Injury
Contact Us About AKI and How VIDAS® NEPHROCHECK® Can Help
Contact Us
References
1. Bianchi NA, Stavart LL, Altarelli M, Kelevina T, Faouzi M, Schneider AG. Association of Oliguria With Acute Kidney Injury Diagnosis, Severity Assessment, and Mortality Among Patients With Critical Illness. JAMA Netw Open. 2021;4(11):e2133094.
2. Kellum JA, Sileanu FE, Murugan R, Lucko N, Shaw AD, Clermont G. Classifying AKI by Urine Output versus Serum Creatinine Level. J Am Soc Nephrol. 2015;26(9):2231-2238.
3. Mehta RL, Cerdá J, Burdmann EA, et al. International Society of Nephrology's 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet. 2015;385(9987):2616-2643.
4. Bagshaw SM, George C, Bellomo R; ANZICS Database Management Committee. Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008;12(2):R47.
5. Ostermann M, Cerdá J. The Burden of Acute Kidney Injury and Related Financial Issues. Contrib Nephrol. 2018;193:100-112.
6. Ostermann M, Joannidis M. Acute kidney injury 2016: diagnosis and diagnostic workup. Crit Care. 2016;20(1):299.
7. Göcze I, Jauch D, Götz M, et al. Biomarker-guided Intervention to Prevent Acute Kidney Injury After Major Surgery: The Prospective Randomized BigpAK Study. Ann Surg. 2018;267(6):1013-1020.
8. Zarbock A, Küllmar M, Ostermann M, et al. Prevention of Cardiac Surgery-Associated Acute Kidney Injury by Implementing the KDIGO Guidelines in High-Risk Patients Identified by Biomarkers: The PrevAKI-Multicenter Randomized Controlled Trial. Anesth Analg. 2021;133(2):292-302.